Apoptosis
Apoptosis/programmed cell death:
Apoptosis is a type of cell death that is induced by a tightly regulated suicide program in which cells destined to die activate intrinsic enzymes that degrade the cells' genomic DNA and nuclear and cytoplasmic proteins.
Causes/examples of apoptosis:
▶Physiological causes:
1) The removal of supernumerary cells (in excess of the required number) during development / programmed cell death during embryogenesis:
Cell death is critical for involution of primordial structures & remodeling of maturing tissues, e.g. during-
- ➤Implantation.
- ➤Organogenesis.
- ➤Developmental involution &
- ➤Metamorphosis.
2) Involution of hormone-dependent tissues on hormone withdrawal: e.g.
- ➤Endometrial cell breakdown during the menstrual cycle.
- ➤ Ovarian follicular atresia in the menopause.
- ➤The regression of the lactating breast after weaning &
- ➤Prostatic atrophy after castration.
- ➤Immature lymphocytes in the bone marrow & thymus.
- ➤B-lymphocytes in the germinal centers that fail to express useful antigen receptors.
- ➤ Epithelial cells in the intestinal crypts.
4) Elimination of potentially harmful self-reactive lymphocytes: To prevent immune reactions against one's own tissues.
5) Death of host cells that have served their useful purpose: Due to withdrawal of survival signals, e.g.
- ➤Neutrophils in an acute inflammatory response &
- ➤ Lymphocytes at the end of an immune response.
▶Pathological causes:
Apoptosis eliminates cells that are injured beyond repair.
1) Apoptosis of injured cell due to DNA damage: By radiation & cytotoxic anti-cancer drugs can damage DNA. Apoptosis of such type of injured cell is a protective mechanism to prevent their conversion into malignant transformation.
2) Apoptosis of cells in which there are accumulation of misfolded proteins: This type of apoptosis occurs in the endoplasmic reticulum (ER stress) due to gene mutation.
3) Cell death in certain infections: Particularly in case of viral infections; e.g. Adenovirus, HIV, hepatitis infections etc.
4) Cell death in tumors.
5) Pathologic atrophy & apoptosis in parenchymal organs after duct obstruction: e.g. in the pancreas, parotid gland & kidney.
▶Morphologic features of apoptosis:
1) Cell shrinkage:
- ➤Cell size: Smaller than normal cell.
- ➤Cytoplasm: Dense.
- ➤ Organelles: Relatively normal but tightly packed.
- ➤Cell membrane: Remain intact during apoptosis, but in the last stage of apoptosis it becomes permeable.
2) Chromatin condensation:
✔ This is the most characteristic feature of apoptosis.
✔ The chromatin aggregates peripherally (under the nuclear membrane) and transformed into dense masses of various shapes and sizes.
✔ The nucleus itself may break up, producing two or more fragments.
3) Formation of cytoplasmic blebs & apoptotic bodies:
The apoptotic cell first shows extensive surface blebbing, then undergoes fragmentation into membrane-bound apoptotic bodies composed of cytoplasm and tightly packed organelles, with or without nuclear fragments.
4) Phagocytosis of apoptotic cells or cell bodies:
✔ Phagocytosis occurs usually by macrophages.
✔ The apoptotic bodies are rapidly ingested by phagocytes and degraded by the phagocyte's lysosomal enzymes.
▶Pathogenesis/ mechanism of apoptosis:
Apoptosis is the endpoint of an energy-dependent cascade of molecular events and results from the activation of enzymes called caspases.
▶Initiation phase/signaling pathways that initiate apoptosis:
During this period, some caspases become catalytically active. Two distinct pathways converge caspase activation, e.g.
a) The intrinsic (mitochondrial) pathway of apoptosis:
- ➤The intrinsic / mitochondrial pathway is the major mechanism of apoptosis.
- ➤It results from increased permeability of the mitochondrial outer membrane with consequent release of death-inducing (pro-apoptotic) molecules from the mitochondrial intermembrane space into the cytoplasm.
- ➤The release of mitochondrial pro-apoptotic proteins is tightly controlled by the BCL2 family of proteins.
- ➤The mitochondrial pathway leads to activation of the initiator caspase-9.
b) Extrinsic/death receptor-initiated pathway of apoptosis:
- ➤This pathway is located in cell membrane & initiated by engagement of plasma membrane death receptors on a variety of cells.
- ➤Death receptors are members of the TNF receptor family & a related protein called Fas that contain a cytoplasmic domain involved in protein-protein interactions that is called the death domain because it is essential for delivering apoptotic signals.
- ➤The death receptor pathway leads to activation of the initiator caspases 8 & 10.
❖ Execution phase:
Caspases trigger the degradation of critical cellular components.
- ➤The enzymatic death program is set in motion by rapid and sequential activation of the executioner caspases (e.g. caspase 3 & 6) act on many cellular components.
- ➤These activated caspases cleave an inhibitor of a cytoplasmic DNase→ make the DNase enzyme active → DNase enzyme induces cleavage of DNA.
- ➤Caspases also degrade structural components of the nuclear matrix and thus promote fragmentation of nuclei.
❖Removal of dead cells: By phagocytosis.
 |
| Figure: Mechanism of apoptosis. |
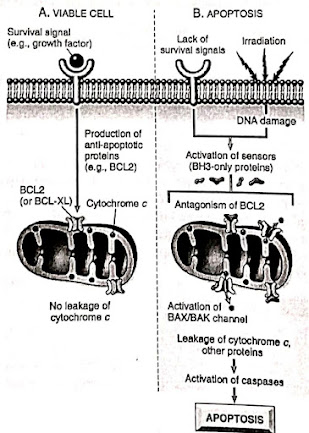 |
| Figure: The intrinsic (mitochondrial) pathway of apoptosis. |
Caspases:
❖They are named so, because they are cysteine proteases that cleave proteins after aspartic residues.
❖Like many proteases, caspases exist as inactive proenzymes, or zymogens.
❖They must undergo enzymatic cleavage to become active.
❖The presence of cleaved, active caspases is a marker for cells undergoing apoptosis.
❖The activation of caspases depends on a finely tuned balance between production of pro- apoptotic and anti-apoptotic proteins.
Caspases/enzymes responsible for apoptosis:
1) Initiation phase:
- ➤Intrinsic / mitochondrial pathway: Caspase 9.
- ➤Extrinsic / cell membrane death receptor pathway: Caspases 8 & 10.
2) Execution phase: Caspase 3 & 6.
Differences between necrosis and apoptosis:
Gangrene
Gangrene: Gangrene means macroscopic death (necrosis) of tissue with superadded putrefaction.
Types:
- Dry gangrene.
- Wet/moist gangrene.
- Gas gangrene: It is a specific moist gangrene caused by Clostridium perfringens in most cases.
❖ Signs of gangrene:
- ✓ Changes of colour: Pale, bluish, purple & finally black.
- ✓ Loss of temperature.
- ✓ Loss of sensation.
- ✓ Loss of pulsation.
- ✓ Loss of function.
❖ Some gangrene-related terms:
- ✓ Noma: A gangrenous lesion of the vulva or mouth (when it is alternatively called cancrum oris) occurring usually in malnourished children after an infectious disease such as measles.
- ✓ Postoperative synergistic gangrene: Which implicates the anterior abdominal wall and thighs.
- ✓ Fournier's gangrene: A fulminating lesion of the scrotum, which is usually completely destroyed, so that the testes are left exposed.
Dry gangrene:
❖ Causes of dry gangrene: Occurs due to lack of arterial blood supply.
1) Changes in arterial wall:
- ✓ Diabetic gangrene (commonest example).
- ✓ Thromboangitis obliterans (Buerger's disease).
- ✓ Atherosclerosis.
- ✓ Arteriosclerosis.
2) Spasm of artery:
- ✓ Raynaud's disease.
- ✓ Ergot poisoning.
3) Obstruction of the lumen of the artery:
- ✓ Thrombosis.
- ✓ Embolism.
4) Pressure effect: Pressure from outside by tumour, tight plaster.
➤Site: Usually occurred in distal part of extremity. Usually, gangrene starts at the great toe.
➤Pathogenesis of dry gangrene:
Dry gangrene occurs due to impairment of the arterial supply, (But venous drainage remains intact)
↓
Due to impairment in the arterial supply, ischaemic coagulative necrosis occurs
↓
The gangrenous area appears cold, dry, shriveled, mummified and black due to iron sulphide and foul smelling
↓
Iron is derived from haemolysed RBC and H2S from putrefaction by involved saprophytes
↓
There is a line of demarcation between necrotic tissue and the healthy inflammatory zone
➤ Zones of dry gangrene: 3 zones of dry gangrene-
- Zone of granulation tissue over necrotic area.
- Zone of inflammation
- Zone of demarcation: It separates necrotic tissue from inflammatory zone formed by contraction of granulation tissue and is the guideline for amputation.
❖ Causes of dry gangrene:
Mnemonic → RESTED
- ➤ R = Raynaud's disease,
- ➤ E = Embolism,
- ➤ S = Senile atherosclerosis,
- ➤ T Thrombosis,
- ➤ E = Ergot poisoning,
- ➤ D= Diabetic arteritis.
Buerger's disease
Buerger's disease/ thromboangitis obliterans:
- ✓ Involves small and medium-sized arteries and veins.ib zomradesenvoll you t2.0
- ✓ Involves the extremities.
- ✓ Recurrent neutrophilic vasculitis with micro-abscess formation.
- ✓ Segmental thrombosis leads to vascular insufficiency.
Vessels affected in Buerger's disease:
❖ Medium and small sized vessels: e.g.
- Dorsalis pedis.
- Posterior and anterior tibialis.
- Radial artery,
- Ulnar &
- Digital artery.
❖ Rarely mesenteric, cerebral and coronary vessels may be affected.
Pathology of the Buerger's disease:
Localized inflammation in the walls of arteries & veins
↓
Thrombosis
↓
Occlusion of the lumen (or obliteration)
↓
Ischaemia, ulceration & gangrene
Wet gangrene
Moist gangrene/wet gangrene:
➤ Sites of wet gangrene:
1) Commonest site: Intestine is the commonest site. Wet gangrene in the intestine occurs in-
- ➤ Strangulated hernia.
- ➤ Intussusception.
- ➤ Volvulus &
- ➤ Trombosis in mesenteric artery.
2) Bed sores.
3) Lungs.
4) Other sites: Vulva, scrotum, anterior abdominal wall, thigh etc.
❖ Pathogenesis of wet gangrene:
It develops due to obstruction of both arterial supply & venous drainage particularly in moist areas
↓
The gangrenous part is moist, blackish and offensive in smell
↓
There is no line of demarcation
➤ Differences between dry gangrene and moist gangrene:




No comments:
Post a Comment